The Infected Blood Inquiry in the UK is due to conclude almost seven years after it was first announced.
But what is the infected blood scandal? Here's the answers to questions on what is considered to be the biggest treatment disaster in the history of the NHS.
What happened?
Tens of thousands of people in the UK were infected with HIV and/or hepatitis after they were given contaminated blood and blood products between the 1970s and early 1990s.
These include people who needed blood transfusions for accidents, in surgery or during childbirth, and patients with certain blood disorders who were treated with donated blood plasma or blood transfusions.
What were the consequences?
It has been estimated that one person dies as a result of infected blood every four days.
Some 3,000 people have died and others have been left with lifelong health complications.
The Inquiry's Report will be published on 20 May.
The Inquiry has just announced further details about the timings of the day. To find out more, read this news story: https://t.co/BOq9YoaIdh— Infected Blood Inquiry (@bloodinquiry) May 9, 2024
Who was affected?
There are two main groups of victims – people who needed blood transfusions and people with bleeding disorders who needed blood, or blood products, as part of their treatment.
People need blood transfusions for a wide variety of reasons, including routine surgery, as a result of childbirth or if they have been in an accident or had an injury where they have lost a lot of blood.
Many victims had bleeding disorders, particularly people with the condition haemophilia.
Haemophilia is an inherited disorder where the blood does not clot properly. Most people with the condition have a shortage of the protein that enables human blood to clot, known as Factor VIII.

In the 1970s, a new treatment was developed – factor concentrate – to replace the missing clotting agent, which was made from donated human blood plasma.
Manufacturers made the product by pooling plasma from tens of thousands of people – increasing the risk of the product containing blood infected with viruses including hepatitis and HIV.
People with haemophilia were treated with British and American blood products.
A shortage of UK-produced factor concentrate meant clinicians relied on imports from the United States, where people in prisons were paid to be donors, despite being at higher risk of carrying infection.
Many patients welcomed this new treatment, which could be delivered by injection at home, as prior to its introduction, patients required transfusions with plasma which had to be given in hospital.
What are the infections people contracted?
Blood-borne infections are viruses that are carried in the blood, such as hepatitis C and human immunodeficiency virus (HIV).
HIV is a virus that damages the cells in the body’s immune system and weakens the ability to fight everyday infections and disease. Aids (acquired immune deficiency syndrome) is the term used to describe a number of potentially life-threatening infections and illnesses that happen when the immune system has been severely damaged by the HIV virus.
Medical advances mean that most people who contract the virus now will live a long and healthy life and most people with HIV will not develop any Aids-related illnesses.
New data from UKHSA shows a large reduction in the number of people living with chronic hepatitis C (HCV) infection in England. Symptoms can go unnoticed for years, but early detection & treatment can help reduce the risk of passing the virus onto others.https://t.co/zJrDSghXwj pic.twitter.com/pvz1kJSQXt
— UK Health Security Agency (@UKHSA) January 30, 2024
Hepatitis C is a virus that is passed on through blood-to-blood contact and infects the liver. Without treatment, it can cause serious damage to the liver.
In 1989, it was first named, having previously been known as “non-A, non-B hepatitis”.
The disease is known as the “silent killer” as some people can live with the virus for many years before realising that they are infected. But the delay in diagnosis can lead to irreparable liver damage.
The Hepatitis C Trust has urged anyone who had a blood transfusion before 1991 to get tested for the virus.
People were infected with other viruses including hepatitis B and a small number contracted Variant Creutzfeldt-Jakob disease.
When was the inquiry announced?
Former UK prime minister Theresa May ordered the inquiry in July 2017 after years of campaigning by victims and their loved ones.
At the time, some 2,400 people had died as a result of the scandal. The number is now estimated to have exceeded 3,000.
Mrs May said the scandal was an “appalling tragedy” which should never have happened.
She said that thousands of patients expected “the world-class care our NHS is famous for, but they were failed”.
A finger prick test is one of the ways to test for #HIV. Symptoms can take years to appear, so if you’re concerned get yourself checked this #NationalHIVTestingWeek and #GiveHIVTheFinger. @THTorguk pic.twitter.com/wxyfsMaWjC
— NHS England (@NHSEngland) November 17, 2018
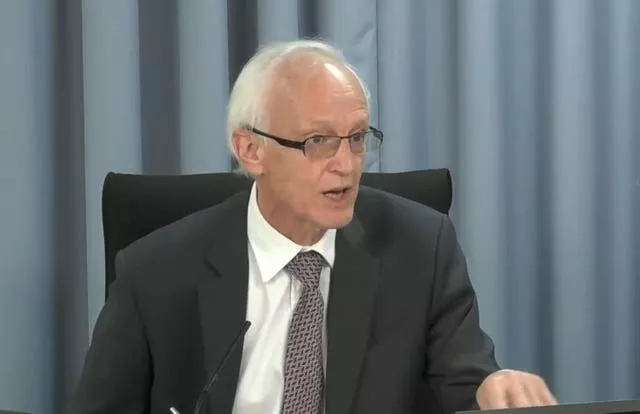
Who is Sir Brian Langstaff?
Former UK High Court judge Sir Brian Langstaff was appointed to chair the inquiry on February 8th, 2018.
He has previous experience working in public inquiries, having served as lead counsel to the Bristol Royal Infirmary inquiry in 1998.
Mr Langstaff has been commended for his compassion by many members of the infected blood community. People infected and affected have said that they expect his report will be balanced and fair.
Today we’re lobbying Parliament - demanding immediate compensation for those infected and affected by contaminated blood. 11 months on from the Public Inquiry’s recommendations and we’re still waiting. #DyingForJustice pic.twitter.com/Ho4Qj3eyz1
— Haemophilia Society (@HaemoSocUK) February 28, 2024
What has the inquiry looked at?
The terms of reference for the inquiry set out a number of issues for it to examine.
These include examining what happened and why; the impact on those affected; the response of the UK government and others; consent; communication and information sharing; the treatment, care and support people received; whether or not there was a cover-up and who was responsible.
As a result of these issues, it is likely that the inquiry chair will make a series of recommendations.
Mr Langstaff heard evidence between 2019 and 2023.
Some 374 people have given oral evidence, and the inquiry has received more than 5,000 witness statements and reviewed more than 100,000 documents.
What about compensation?
The UK government is now working at pace to get an arms-length compensation body set up, having faced criticism in the past over the speed at which it responded to calls for action on compensation.
Interim compensation payments of £100,000 have been made to around 4,000 infected people or bereaved partners.
UK ministers recently announced that these interim payments would be extended to the “estates of the deceased”.







