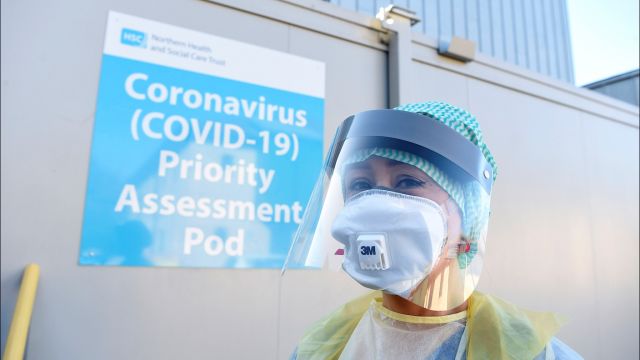
Pandemic-related pressure on hospitals in Northern Ireland has been building, with patients unable to enter emergency departments left waiting in ambulances due to social distancing limitations.
Pressure on hospitals across the region has been increasing and made more complicated due to Covid-19, the Director of Operations for the Northern Health and Social Care Trust has said.
Wendy Magowan told RTÉ radio’s Morning Ireland that services in the system have been impacted because of the rise in Covid-19 cases.
It was confirmed yesterday that two patients and seven members of staff in a ward at the Ulster Hospital in Belfast had tested positive for the virus.
It has also been reported that non-Covid healthcare services in Irish hospitals may need to be cancelled to facilitate critical care cases from Northern Ireland.
Ms Magowan acknowledged concern expressed by emergency department staff on Monday as people who required admission to Antrim Hospital were left outside in ambulances.
It's incredibly distressing, no one wants to delay anyone in an ambulance. Ambulances need to be out on the ground caring for patients
“Sadly the pressure still there this morning, we had 27 people waiting for beds yesterday afternoon, this morning there is 35 in the emergency department with 33 of those actually waiting for beds,” she said.
“That is a ward that the emergency department is taking care of and there is no capacity in the hospital.
“That's ok now at this time of the morning, but as we move into the day and as we get more referrals and as our GP colleagues start to send patients in and ambulances arrive, that pressure will sadly build again as the day progresses,” she added.
Staffing
Ms Magowan said ambulances were unable to offload patients into crowded emergency departments due to current infection control risks.
“It's incredibly distressing, no one wants to delay anyone in an ambulance. Ambulances need to be out on the ground caring for patients, they do not need to be sitting outside emergency departments,” she said.
“We have one workforce and it is being spread quite thinly - to the extent that we have to move staff to the areas of greatest need.
“Obviously that has an impact on the services we have to deliver, we are absolutely committed to continue our cancer surgery but there are other elements that have had to be stood back to allow staff to go to the areas of need.”
Ms Magowan warned that with the level of sustained community transmission, and as staff live in the community “they are equally as vulnerable to contracting or being in contact with Covid in the community”.
“With track and trace we do have significant number of staff self-isolating and that again impacts on our services,” she said.