The Irish healthcare system cannot rely on other countries to solve the hospital waiting list crisis, said the Bishop of Limerick, as he launched a €210 million plan to expand the Treaty City’s St John’s Hospital.
The bishop said Irish public patients should not be expected to travel to receive scheduled care, as it emerged last week that a new hospital opened in Spain to be used for treating patients on long public waiting lists in Ireland.
The hospital, in Alicante, is a part of a major new healthcare agreement, where patients are to be treated under the EU Cross Border Directive, with the Health Service Executive (HSE) covering the price of treatment up to the cost it would be in Ireland, but not the patients travel or private expenses.
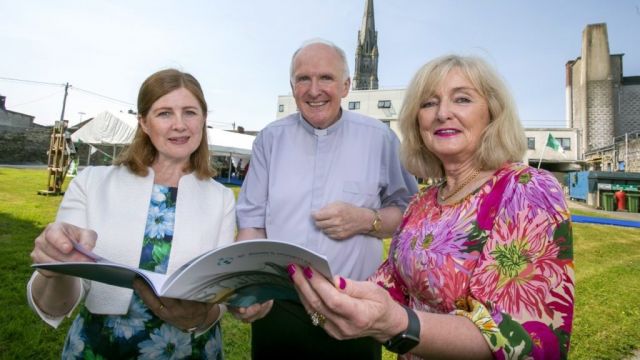
Bishop Brendan Leahy, who is Chair of the Board of St John’s, said: “The future generations are calling us here today to do what we can to ensure that they won't have to travel to Galway or Cork, or indeed Spain, to receive scheduled surgery and the excellent care possible in a newly energised St John's.”
Five-year expansion strategy
Management at the hospital, which founded in 1780, unveiled a five-year expansion strategy, Monday, including a 150-bed on site extension “to ensure best-in-class care delivered at hospital is matched by state-of-the-art facilities”.
The plan, developed by the UL Hospitals Group in consultation with staff and local GPs, is seen as playing a “key role in addressing capacity requirements in the Mid-West”, stated St John’s.
“The proposal addresses the necessary capacity requirement to tackle public waiting lists by accommodating a very significant proportion of the scheduled care work in the region, and it provides solutions to the critical needs associated with the public waiting lists.”
“St John’s already has the sixth-busiest endoscopy list and 12th busiest elective surgery list in the country, as well as the second-busiest Injury Unit in the country.”
“Among the strategy priorities identified in the consultation process are the development of a new modern €60m facility complete with increased single ensuite rooms, greater access to services, development of services for the management of chronic diseases and provision of seven-day injury unit services.”
Bed capacity
The proposed development will increase St John’s bed capacity from an 89 to 200 and aims to deliver an additional 31,390 bed days per annum in the Limerick region.
It will “also deliver a safer patient environment, increase in-patient access by 150 per cent, and provide an overall improvement in patient experience as well as staff working experience”.
A total of 667 additional full time equivalent jobs, via direct and indirect employment, are proposed, including 52 new frontline clinicians and support roles at St Johns, which presently employs 350 staff.
If approved, the development will take an estimated 36 months to complete.
St John’s chief executive, Emer Martin, said, despite providing “outstanding results” to patients for over two centuries, it has “been long since acknowledged that the facilities here are simply not fit for the purpose or the people”.
Bishop Leahy agreed that it makes “absolute sense to not alone address the shortcomings in the existing hospital but, in doing so, give more people access to this standard of care in the Mid-West”.
“We have the capacity on the site to do this and in a region that clearly needs key solutions like this to help address pressures on the system,” added the Bishop.
Patient overcrowding
Full time Accident & Emergency departments at St Johns, Ennis Hospital and Nenagh Hospital were downgraded to University Hospital Limerick in 2009, however, the increased pressure on UHL has exacerbated patient overcrowding in the region.
Last month the UL Hospitals Group said it accepted the findings of a damning report by the Health and Information and Quality Authority (HIQA), which found “insufficient” nursing staff numbers at the city’s University Hospital Limerick was “having an impact on the safe provision of care”, and its “overcrowded and understaffed emergency department posed a significant risk” to patients.
The group’s Chief Clinical Director, Professor Brian Lenehan, apologised to patients and families and acknowledged UHL’s responses to overcrowding were “not sufficient to meet the unprecedented increase in demand on our service”.
However, Prof Lenehan said UHL had “fewer inpatient beds and fewer consultants and NCHDs to provide care than comparable hospitals, and serves a region with a higher frailty index and a city with a higher deprivation index”.
He added “the growth in demand on our hospital since the pandemic has also been disproportionate and exceptional” when compared to other hospitals.