A US health panel says it is time to resume use of Johnson & Johnson’s Covid-19 vaccine, despite a very rare risk of blood clots.
Out of nearly eight million people vaccinated before the US suspended using J&J’s shot, health officials uncovered 15 cases of a highly unusual kind of blood clot, three of them fatal. All were women, most younger than 50.
Advisers to the Centres for Disease Control and Prevention said while J&J’s vaccine is important for fighting the pandemic, it is also critical that younger women be told about that risk in clear, understandable terms — so they can decide if they would rather choose an alternate vaccine instead.
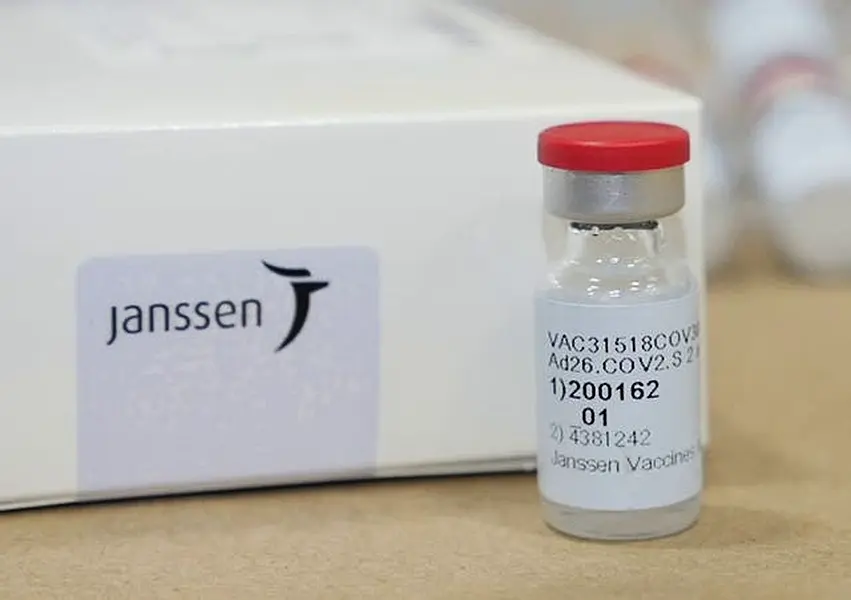
The panel voted 10-4 to lift an 11-day pause in use of the J&J shot while adding warnings that women and health workers would see in leaflets at vaccination clinics.
The group debated, but ultimately steered clear of outright age restrictions.
“This is an age group that is most at risk (of the clotting) that is getting vaccine predominately to save other peoples’ lives and morbidity, not their own. And I think we have a responsibility to be certain that they know this,” said Dr Sarah Long of Drexel University College of Medicine, who voted against the proposal because she felt it did not go far enough in warning women.
The CDC and Food and Drug Administration will weigh Friday’s recommendation in deciding whether to end the pause; the CDC typically follows the recommendation of its advisers and CDC Director Dr Rochelle Walensky has promised swift action.
European regulators earlier this week made a similar decision, saying the clot risk was small enough to allow the rollout of J&J’s shot.
At issue is a kind of blood clot that forms in unusual places, such as veins that drain blood from the brain, and in patients with abnormally low levels of the platelets that form clots.
The CDC and Food and Drug Administration initially spotted six people who developed such clots one to three weeks after J&J vaccination. On Friday, health officials said nine more cases came to light in the last week or so.
The needle-in-a-haystack reports raised alarm because European regulators already had uncovered similar rare clots among recipients of another Covid-19 vaccine, from AstraZeneca.
The AstraZeneca and J&J shots, while not identical, are made with the same technology.
European scientists found clues that an abnormal platelet-harming immune response to AstraZeneca’s vaccine might be to blame – and if so, then doctors should avoid the most common clot treatment, a blood thinner called heparin.
That added to US authorities’ urgency in pausing J&J vaccinations so they could tell doctors how to diagnose and treat these rare clots. Several initial patients were treated with heparin before anyone realised that might harm instead of help.
Two-dose vaccines from Pfizer and Moderna, which are made differently and have not been linked to clot risks, are the mainstay of the US vaccination effort.
But J&J mass vaccination clinics were cancelled after the April 13 pause, and many states had been counting on the one-and-done option to also help protect hard-to-reach populations including people who are homeless or disabled.







